What Is Insurance Prior Authorization for GLP-1s?
Insurance prior authorization for GLP-1 medications is a process where insurance companies require approval before covering the cost of these treatments. This step ensures that the prescribed GLP-1 medication is medically necessary and appropriate for the patient’s condition. Dr. Leah Joseph, MD at JosephCareRX, is here to assist patients in understanding and managing insurance prior authorization for GLP-1s, ensuring smoother access to the medication. For more information, contact us or book an appointment online. We are conveniently located at 2504 Raeford Road #101 Fayetteville NC 28305.
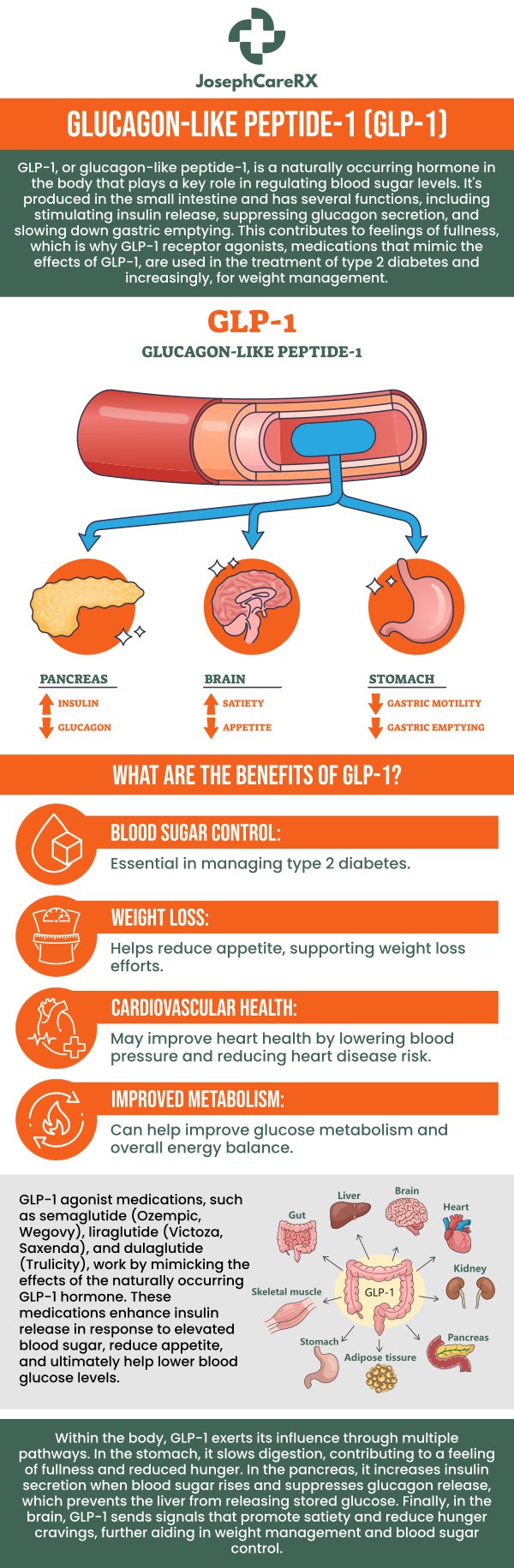
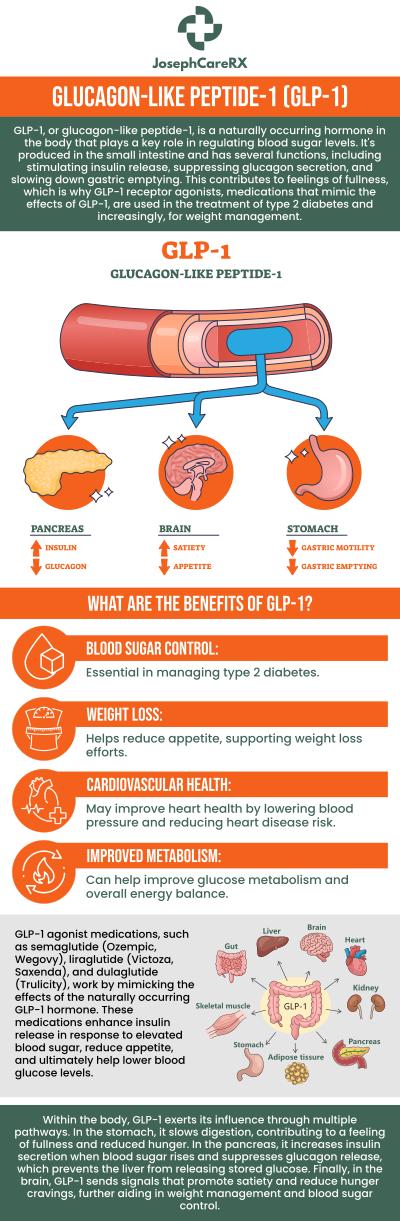
Table of Contents:
What is insurance prior authorization for GLP-1s?
Why is prior authorization required for GLP-1s?
How do I request prior authorization for a GLP-1 medication?
What information is needed for prior authorization from Dr. Leah Joseph, MD?
How long does it take for insurance to approve prior authorization for GLP-1s?
Insurance prior authorization for GLP-1 medications is a process that requires approval from your insurance company before the medication can be covered. GLP-1 medications, such as semaglutide (Wegovy) or liraglutide (Saxenda), are often used for weight loss and managing type 2 diabetes, but they can be expensive. In many cases, insurance companies require prior authorization to ensure that the prescribed medication meets their criteria for coverage.
The prior authorization process involves your healthcare provider submitting a request to the insurance company, which includes relevant medical information about your condition. This request helps the insurance company determine if the medication is medically necessary and appropriate for your treatment. Without prior authorization, the medication may not be covered by your insurance plan, and you may be responsible for paying out-of-pocket.
At JosephCareRX, our team works closely with her patients to handle the prior authorization process for GLP-1 medications. We ensure that the necessary documentation is submitted, helping patients receive the medications they need for effective weight management and diabetes care.
Prior authorization is required for GLP-1 medications to ensure that they are medically necessary and that the insurance company is covering treatments that align with their approved guidelines. Insurance companies often have specific criteria for covering medications like GLP-1s, especially since they are considered specialty drugs and can be costly. By requiring prior authorization, insurers aim to:
● Ensure the appropriate use of expensive medications.
● Confirm that the prescribed medication is necessary based on the patient’s medical history, symptoms, and condition.
● Prevent misuse or overprescription of certain treatments.
For GLP-1 medications, insurers may require evidence that the patient has tried other treatments or that the medication is essential for managing weight loss in the presence of other conditions like type 2 diabetes, hypertension, or cardiovascular disease.
At JosephCareRX, our team emphasizes that prior authorization is an important part of the process to ensure that the patient’s treatment is effective, necessary, and covered by insurance. The documentation process helps streamline access to the right care, without delays in treatment.
To request prior authorization for a GLP-1 medication, you and your healthcare provider must work together to submit a formal request to your insurance company. Here’s a general process to follow:
● Consult with your healthcare provider: If Dr. Leah Joseph, MD, determines that a GLP-1 medication is appropriate for your condition, she will initiate the prior authorization request.
● Submit required medical documentation: Your provider will need to submit supporting medical documentation to demonstrate why the GLP-1 medication is necessary for your treatment. This may include medical history, treatment records, and evidence of other treatments you’ve tried.
● Insurance review: The insurance company will review the request and documentation to determine if the medication meets their approval criteria. This may take a few days to weeks.
● Approval or denial: Once reviewed, the insurance company will either approve or deny the request. If denied, your healthcare provider may appeal the decision or recommend alternative treatments.
At JosephCareRX, we ensure that prior authorization requests for GLP-1 medications are thoroughly prepared, increasing the likelihood of quick and successful approval.
For prior authorization to be approved for a GLP-1 medication, we will need to provide specific information about your medical condition and treatment history. The required information typically includes:
● Diagnosis: Documentation of the patient’s condition, such as type 2 diabetes, obesity, hypertension, or cardiovascular issues, that warrants the use of a GLP-1 medication.
● Previous treatments: Information on any other weight loss or diabetes treatments you’ve previously tried, including medications, diet, and exercise programs.
● Medical history: Relevant history related to metabolic health, insulin resistance, or other conditions that might make GLP-1 therapy appropriate.
● Current medications: A list of other medications being taken, to ensure there are no interactions and that the GLP-1 therapy is the most appropriate option.
● Clinical evidence: Any lab results, such as A1C levels, blood pressure readings, or BMI measurements, that support the necessity of the medication.
At JosephCareRX, we ensure that all necessary documentation is included in the prior authorization request, making the process as smooth and efficient as possible. This ensures timely access to treatment and coverage from your insurance provider.
The time it takes for insurance companies to approve a prior authorization for GLP-1 medications can vary. Typically, it takes anywhere from 7 to 14 days for the insurance company to review the request and make a decision. However, this timeline can be longer, depending on the complexity of the case or the need for additional information.
If the insurance company requires further clarification or documentation, the approval process can take longer. In some cases, the request may be denied, in which case the healthcare provider can appeal the decision, which may add additional time to the process.
To expedite the process, Dr. Leah Joseph, MD, and her team at JosephCareRX ensure that all the necessary information is submitted correctly and promptly. This helps avoid delays and ensures that patients can begin their GLP-1 therapy without unnecessary interruptions. For more information, contact us or book an appointment online. We are conveniently located at 2504 Raeford Road #101 Fayetteville NC 28305. We serve patients from Fayetteville, NC, Hope Mills NC, Spring Lake NC, Cedar Creek NC, Woodbridge NC, Pinehurst NC and surrounding areas, We also offer virtual only visits in select states nationwide.
Check Out Our 5 Star Reviews